Shailender Kumar Hooda
Most countries in the world
spend a sizable amount of public fund on health, though delivery of health
services is organised through a mix of government and private providers. The countries recording high level of public
spending in health have secured better health outcomes compared to the
countries with low spending, barring few exceptions like the US, where high
public spending co-exists with high exclusion. Some however have also managed
better outcomes with little public funds while improving allocation of funds,
better management and effective service delivery mechanisms (NCMH, 2005). India’s
performance in improving the health outcomes, even after announcement of more
than 21 committees and commissions on health sector reforms, has remained far
from satisfactory levels. For instance, some of the health outcomes (infant,
child and maternal mortality rates) are not only lower than the Millennium
Development Goal targets but even worse than some of the developing countries.
The infant mortality rates (IMR) of India
is around 54 whereas Sri
Lanka’s IMR is 17 (WHR, 2010). The life
expectancy at birth (64 years) of an average Indian is at least 15 years lower
than that of developed countries and even lower than the neighbouring Sri Lanka (74
years). Almost half of Indian children suffer from malnutrition which is even worse
than what recorded in some places in Sub-Saharan Africa. More than 50 per cent
of women suffer from anaemia (WHR, 2010). The rural-urban gaps in health
outcomes are not only persisting but have widened over the years. In order to
understand this unsatisfactory performance in the health sector, one needs to
look at the gap between health policy commitments by the government and the
allocation of funds in respective segments.
spend a sizable amount of public fund on health, though delivery of health
services is organised through a mix of government and private providers. The countries recording high level of public
spending in health have secured better health outcomes compared to the
countries with low spending, barring few exceptions like the US, where high
public spending co-exists with high exclusion. Some however have also managed
better outcomes with little public funds while improving allocation of funds,
better management and effective service delivery mechanisms (NCMH, 2005). India’s
performance in improving the health outcomes, even after announcement of more
than 21 committees and commissions on health sector reforms, has remained far
from satisfactory levels. For instance, some of the health outcomes (infant,
child and maternal mortality rates) are not only lower than the Millennium
Development Goal targets but even worse than some of the developing countries.
The infant mortality rates (IMR) of India
is around 54 whereas Sri
Lanka’s IMR is 17 (WHR, 2010). The life
expectancy at birth (64 years) of an average Indian is at least 15 years lower
than that of developed countries and even lower than the neighbouring Sri Lanka (74
years). Almost half of Indian children suffer from malnutrition which is even worse
than what recorded in some places in Sub-Saharan Africa. More than 50 per cent
of women suffer from anaemia (WHR, 2010). The rural-urban gaps in health
outcomes are not only persisting but have widened over the years. In order to
understand this unsatisfactory performance in the health sector, one needs to
look at the gap between health policy commitments by the government and the
allocation of funds in respective segments.
Commitments Vs Achievements
Since independence, India followed
a welfare state approach with healthcare falling under the auspices of the
government. Healthcare was supposed to be the responsibility of central and
state governments, particularly in determining priorities, financing and
delivery of health services to the general population. The recommendations of
first Health Planning and Development Committee (Bhore Committee, 1946) report,
that emphasised the development of basic infrastructure and manpower, were
taken up in the First (1951-56) and the
Second (1956-61) Five-Year plans of India. Data shows that prescribed
norms of health infrastructure could not be met even after sixty years of
independence, in 2010. Under the Community Development Programme (1951-55), India formulated
a plan to achieve one PHC (Primary Health Centre) per one lakh population, but
the achievement is around one-fifth (one PHC per 5.5 lakh population) of the
targets set for the year 2010. Surprisingly, based on the recommendations of
various committees and Alma-Ata declaration
(1978), India
announced its first formal National Health Policy (NHP) in 1983. NHP pledged to
achieve ‘Health for all by the year 2000’, the primary vehicles conceived were
introduction of certain numbers of CHCs (Community Health Centre), PHCs and SCs
(Sub-centres) in the country. A shortfall of 4372 CHCs, 1875 PHCs and 10992 SCs
was noticed in 2001. Furthermore, as per Indian Public Health Standard (IPHS),
there should be 4-6 beds and 30 beds in each PHC and CHC respectively. In 2010,
only 59 per cent of the PHCs and 72 per cent of the CHCs could achieve the
prescribed standard. Thus the physical and human infrastructure in the health
sector in India
grossly falls short of the prescribed norms.
a welfare state approach with healthcare falling under the auspices of the
government. Healthcare was supposed to be the responsibility of central and
state governments, particularly in determining priorities, financing and
delivery of health services to the general population. The recommendations of
first Health Planning and Development Committee (Bhore Committee, 1946) report,
that emphasised the development of basic infrastructure and manpower, were
taken up in the First (1951-56) and the
Second (1956-61) Five-Year plans of India. Data shows that prescribed
norms of health infrastructure could not be met even after sixty years of
independence, in 2010. Under the Community Development Programme (1951-55), India formulated
a plan to achieve one PHC (Primary Health Centre) per one lakh population, but
the achievement is around one-fifth (one PHC per 5.5 lakh population) of the
targets set for the year 2010. Surprisingly, based on the recommendations of
various committees and Alma-Ata declaration
(1978), India
announced its first formal National Health Policy (NHP) in 1983. NHP pledged to
achieve ‘Health for all by the year 2000’, the primary vehicles conceived were
introduction of certain numbers of CHCs (Community Health Centre), PHCs and SCs
(Sub-centres) in the country. A shortfall of 4372 CHCs, 1875 PHCs and 10992 SCs
was noticed in 2001. Furthermore, as per Indian Public Health Standard (IPHS),
there should be 4-6 beds and 30 beds in each PHC and CHC respectively. In 2010,
only 59 per cent of the PHCs and 72 per cent of the CHCs could achieve the
prescribed standard. Thus the physical and human infrastructure in the health
sector in India
grossly falls short of the prescribed norms.
The second National Health
Policy which was announced in 2002, itself recognised that the performance of
first NHP is unsatisfactory particularly because of low level of government
spending. The second NHP recommended that government spending in health should
increase (i) from its existing level from about 0.9 per cent of GDP to 2 per
cent of GDP and (ii) from existing level of about 5.5 per cent of total budget
spending to 8 per cent of total budget spending by the year 2010. In 2010, the
level of spending recorded to be around 1.09 per cent of GDP which is
significantly lower than the commitments. In 2004-05, the National Commission of
Macro-Economic and Health (NCMH, 2005) of India estimated required level of
resource that need to be spent by every state government to meet the adequate
level of basic health services in the country by the end of 2009-10. An
analysis of the required level of resources against the actual allocation shows
that most of the state governments could not achieve the prescribed level of
health spending during the specified period. Except for Himachal Pradesh, there
exist high gaps between required resources and actual spending in most states (Figure-1). Such gaps in resource
requirements were not only noticed in low income states like Bihar, Orissa,
Rajasthan and Uttar Pradesh but the high income states like Punjab and Maharashtra could not maintain the required level of
spending.
Policy which was announced in 2002, itself recognised that the performance of
first NHP is unsatisfactory particularly because of low level of government
spending. The second NHP recommended that government spending in health should
increase (i) from its existing level from about 0.9 per cent of GDP to 2 per
cent of GDP and (ii) from existing level of about 5.5 per cent of total budget
spending to 8 per cent of total budget spending by the year 2010. In 2010, the
level of spending recorded to be around 1.09 per cent of GDP which is
significantly lower than the commitments. In 2004-05, the National Commission of
Macro-Economic and Health (NCMH, 2005) of India estimated required level of
resource that need to be spent by every state government to meet the adequate
level of basic health services in the country by the end of 2009-10. An
analysis of the required level of resources against the actual allocation shows
that most of the state governments could not achieve the prescribed level of
health spending during the specified period. Except for Himachal Pradesh, there
exist high gaps between required resources and actual spending in most states (Figure-1). Such gaps in resource
requirements were not only noticed in low income states like Bihar, Orissa,
Rajasthan and Uttar Pradesh but the high income states like Punjab and Maharashtra could not maintain the required level of
spending.
In 2005, central government
launched a flagship programme called National Rural Health Mission-NRHM. The Mission has set an
ambitious goal of increasing in government spending in health to 2-3 per cent
of GDP by 2012. But spending remained 1.2 per cent of GDP at the end of 11th
Plan (2012). Even after adding the expenditure of complementary (water supply
and sanitation) services, the spending hovered around 1.6 per cent of GDP which
is less than the commitment. The failure in various policy commitments reflects
that India,
despite having low health outcomes fails to allocate resources that increase
provisions for health care. Overall, neither the Primary Health Care approach,
‘Health for All’ targets nor the spending commitment ever been implemented and fulfilled
in the country. This reflects that health has always been a low priority sector
in India.
Recently, the High level Expert Groups (2012) on Universal Health Coverage has
proposed to increase the government (central and state combined) spending in
health from the current level of 1.2 per cent of GDP to at least 2.5 per cent
by the end of the 12th Plan and to at least 3 per cent of GDP by
2022. Past experience however leaves little hope in fulfilling these
commitments.
launched a flagship programme called National Rural Health Mission-NRHM. The Mission has set an
ambitious goal of increasing in government spending in health to 2-3 per cent
of GDP by 2012. But spending remained 1.2 per cent of GDP at the end of 11th
Plan (2012). Even after adding the expenditure of complementary (water supply
and sanitation) services, the spending hovered around 1.6 per cent of GDP which
is less than the commitment. The failure in various policy commitments reflects
that India,
despite having low health outcomes fails to allocate resources that increase
provisions for health care. Overall, neither the Primary Health Care approach,
‘Health for All’ targets nor the spending commitment ever been implemented and fulfilled
in the country. This reflects that health has always been a low priority sector
in India.
Recently, the High level Expert Groups (2012) on Universal Health Coverage has
proposed to increase the government (central and state combined) spending in
health from the current level of 1.2 per cent of GDP to at least 2.5 per cent
by the end of the 12th Plan and to at least 3 per cent of GDP by
2022. Past experience however leaves little hope in fulfilling these
commitments.
Figure-1: Resource
Requirements vs. Actual Health Spending across Indian States
Requirements vs. Actual Health Spending across Indian States
Multifaceted
NRHM Initiatives: A Critique
NRHM Initiatives: A Critique
As per the Constitution, health
is a state subject in India.
The state governments would deliver adequate health services to meet the health
need of the population. The central government, however, can directly intervene
in establishing major hospitals and to assist medical education and research.
Another way to intervene in health sector by the central government is to
initiate Central Plan (CPS) and Centrally Sponsored Schemes (CSS), which are generally
implemented through state budgets. Thus the responsibility of fulfilling the
health needs of the population is largely being shifted to the state
governments. In 2005, it was realised that there is high gap in health outcomes
and facilities across Indian states. In order to fill such gap, the central
government, under the NRHM, identified states with high fertility and mortality
rates and otherwise. The former states were named as high focused states-HFS (namely
Assam, Bihar,
Himachal Pradesh, Madhya Pradesh, Orissa, Rajasthan and Uttar Pradesh including
north-eastern states) and the rest are non-high focused states (Non-HFS). Under
NRHM, the promise was made to devolve/transfer more central funds towards HFS
to remove variation in health spending across states and to ensure better (up
to the MDGs) health standards in the country. Evidence however shows that the share
of fund allocation remained lower than the commitments made by central
government. Surprisingly, the ratio of actual fund allocation to commitment – a
high ratio reflecting low priority – found high (around 18 percent) in high
focused states as compared to around 15 percent in non-HFS. Even though it was mandated
that the priority should be accorded to high focused states, the outcome was
the opposite.
is a state subject in India.
The state governments would deliver adequate health services to meet the health
need of the population. The central government, however, can directly intervene
in establishing major hospitals and to assist medical education and research.
Another way to intervene in health sector by the central government is to
initiate Central Plan (CPS) and Centrally Sponsored Schemes (CSS), which are generally
implemented through state budgets. Thus the responsibility of fulfilling the
health needs of the population is largely being shifted to the state
governments. In 2005, it was realised that there is high gap in health outcomes
and facilities across Indian states. In order to fill such gap, the central
government, under the NRHM, identified states with high fertility and mortality
rates and otherwise. The former states were named as high focused states-HFS (namely
Assam, Bihar,
Himachal Pradesh, Madhya Pradesh, Orissa, Rajasthan and Uttar Pradesh including
north-eastern states) and the rest are non-high focused states (Non-HFS). Under
NRHM, the promise was made to devolve/transfer more central funds towards HFS
to remove variation in health spending across states and to ensure better (up
to the MDGs) health standards in the country. Evidence however shows that the share
of fund allocation remained lower than the commitments made by central
government. Surprisingly, the ratio of actual fund allocation to commitment – a
high ratio reflecting low priority – found high (around 18 percent) in high
focused states as compared to around 15 percent in non-HFS. Even though it was mandated
that the priority should be accorded to high focused states, the outcome was
the opposite.
Under NRHM, under fund
devolution criteria, the central government asked the state to increase their
own spending at a specified rate in tandem with increased central funding. It
was found that state governments are failing in their capacity to absorb the
funds that are allocated by central government. The share of unspent amount
with the state as a ratio of total funds released by central government is
recorded around 6.4 per cent and 12.5 per cent for high focused and non-high
focused states respectively, indicating inadequate absorptive capacity of states
to utilize the fund properly. The absorptive capacity however found to be high
in high focused states compared to the non-high focused states which seem to be
a positive indication. The fund absorptive capacity is noticed to be highly
inadequate in West Bengal and Punjab, where
around 56 per cent and 48 per cent of the funds respectively have not been
utilized. It can be argued that lack of inadequate availability of human
resources, weak capacity to plan and execute plans are plausible reasons for
the state governments failing to absorb the central fund adequately.
devolution criteria, the central government asked the state to increase their
own spending at a specified rate in tandem with increased central funding. It
was found that state governments are failing in their capacity to absorb the
funds that are allocated by central government. The share of unspent amount
with the state as a ratio of total funds released by central government is
recorded around 6.4 per cent and 12.5 per cent for high focused and non-high
focused states respectively, indicating inadequate absorptive capacity of states
to utilize the fund properly. The absorptive capacity however found to be high
in high focused states compared to the non-high focused states which seem to be
a positive indication. The fund absorptive capacity is noticed to be highly
inadequate in West Bengal and Punjab, where
around 56 per cent and 48 per cent of the funds respectively have not been
utilized. It can be argued that lack of inadequate availability of human
resources, weak capacity to plan and execute plans are plausible reasons for
the state governments failing to absorb the central fund adequately.
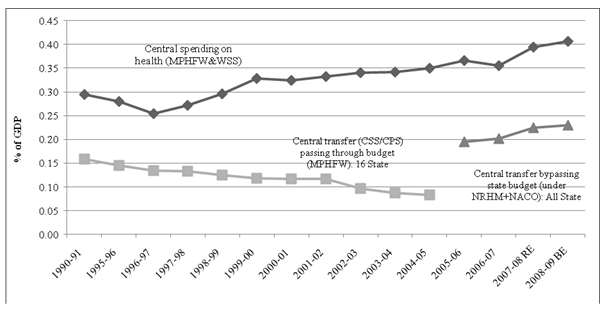
One interesting observation is
that the direction of funds transfer from centre to state has changed
significantly with the implementation of NRHM. Specifically, some of the
central government funds, which were earlier routed through state budget under
the centrally sponsored schemes (CSS) and plan schemes (CPS), now bypasses the
state budgets and are designed to be implemented through state implementing
agencies like State Health Society. Note that the central transfer to states
through CSS/CPS is an important policy initiative of the central government to
support various health programmes running in the state. This helps in meeting
the recurring and non-recurring requirement of these programmes, especially the
programmes related to communicable and non-communicable diseases such as
trachoma, blindness control programmes, family welfare programmes and the
others. With this changing route of central transfer not only it becomes
difficult to comprehend the total government (centre and state) health
expenditure but also entails larger implications for health programmes
initiated by central government. Interestingly central government spending on CSS
and CPS taken together declined from 0.16 per cent of GDP in 1990-91 to 0.08
per cent of GDP in 2004-05 (Figure-2).
This declining share has reduced the budgetary resources provided for dealing
with several existing major communicable and non-communicable diseases and
family welfare programmes. This raises the question of sustainability of some
of the health programmes. Ideally, the long-term sustainability of any one or
all of these central sponsored health programmes, to a large extent, depends on
continuous funding from central government. The declining trends or
uncertainties in resource flows from centre to state would certainly affect the
implementation process and effectiveness of these programs at the state level
and more particularly the needy (poorer) states. This probably indicates that
state governments have to bear most of the burden of health expenditure to
finance these programmes from their own resources.
that the direction of funds transfer from centre to state has changed
significantly with the implementation of NRHM. Specifically, some of the
central government funds, which were earlier routed through state budget under
the centrally sponsored schemes (CSS) and plan schemes (CPS), now bypasses the
state budgets and are designed to be implemented through state implementing
agencies like State Health Society. Note that the central transfer to states
through CSS/CPS is an important policy initiative of the central government to
support various health programmes running in the state. This helps in meeting
the recurring and non-recurring requirement of these programmes, especially the
programmes related to communicable and non-communicable diseases such as
trachoma, blindness control programmes, family welfare programmes and the
others. With this changing route of central transfer not only it becomes
difficult to comprehend the total government (centre and state) health
expenditure but also entails larger implications for health programmes
initiated by central government. Interestingly central government spending on CSS
and CPS taken together declined from 0.16 per cent of GDP in 1990-91 to 0.08
per cent of GDP in 2004-05 (Figure-2).
This declining share has reduced the budgetary resources provided for dealing
with several existing major communicable and non-communicable diseases and
family welfare programmes. This raises the question of sustainability of some
of the health programmes. Ideally, the long-term sustainability of any one or
all of these central sponsored health programmes, to a large extent, depends on
continuous funding from central government. The declining trends or
uncertainties in resource flows from centre to state would certainly affect the
implementation process and effectiveness of these programs at the state level
and more particularly the needy (poorer) states. This probably indicates that
state governments have to bear most of the burden of health expenditure to
finance these programmes from their own resources.
Figure-2:Changing Pattern of Central Transfer to States: Pre
and Post NRHM Analysis
and Post NRHM Analysis
The central spending on NRHM
components that are supposed to be bypassing the state budget and implemented
through state’s autonomous agencies as per cent to GDP has increased during the
period 2005-06 to 2008-09 (Figure-2).
The increasing trend in health expenditure under NRHM, routed through
decentralized agencies, raise doubts about how the implementing agencies will
utilize the transferred funds.
components that are supposed to be bypassing the state budget and implemented
through state’s autonomous agencies as per cent to GDP has increased during the
period 2005-06 to 2008-09 (Figure-2).
The increasing trend in health expenditure under NRHM, routed through
decentralized agencies, raise doubts about how the implementing agencies will
utilize the transferred funds.
As regards to the
sustainability of central sponsored (CSS/CPS) programmes, it has been realised
that NRHM consists of some new schemes but repackages many of the existing
health schemes which are now bypassing the state budget. For instance, the
National Disease Control Programmes (NDCP) which was earlier with the
Department of Health has now been made part of the NRHM. Similarly, the earlier
schemes of the Department of Family Welfare such as reproductive and child
health programme (RCH), immunisation, contraception, information education and
communication (IEC), training and research, area projects and other family
welfare services, are all included in the NRHM. The new initiatives under the
NRHM are mostly financed through what is called the ‘mission flexible pool’
which provides for activities like selection and training of a new cadre of
community health worker called Accredited Social Health Activist (ASHA),
up-gradation of health facilities (community health centre and public health centres)
to first referral units (FRU) and facilities meeting the new Indian Public
Health Standards (IPHS), constitution of patient welfare committees called Rogi Kalyan Samiti (RKS) and district
hospital management committees, mobile medical units, united funds for
sub-centres, preparation of district action plans and so forth. There have also
been some changes in the centrally sponsored schemes now falling under the NRHM
umbrella. The earlier RCH programme (RCH1) funded a fixed set of activities.
Under the NRHM, the earlier form of the RCH programme is being phased out. In
RCH2, most activities are funded through an RCH flexible pool which supports
decentralized planning and flexible programming by the states (NRHM, 2005). All
these show that NRHM includes many schemes covered under the CSS/CPS.
sustainability of central sponsored (CSS/CPS) programmes, it has been realised
that NRHM consists of some new schemes but repackages many of the existing
health schemes which are now bypassing the state budget. For instance, the
National Disease Control Programmes (NDCP) which was earlier with the
Department of Health has now been made part of the NRHM. Similarly, the earlier
schemes of the Department of Family Welfare such as reproductive and child
health programme (RCH), immunisation, contraception, information education and
communication (IEC), training and research, area projects and other family
welfare services, are all included in the NRHM. The new initiatives under the
NRHM are mostly financed through what is called the ‘mission flexible pool’
which provides for activities like selection and training of a new cadre of
community health worker called Accredited Social Health Activist (ASHA),
up-gradation of health facilities (community health centre and public health centres)
to first referral units (FRU) and facilities meeting the new Indian Public
Health Standards (IPHS), constitution of patient welfare committees called Rogi Kalyan Samiti (RKS) and district
hospital management committees, mobile medical units, united funds for
sub-centres, preparation of district action plans and so forth. There have also
been some changes in the centrally sponsored schemes now falling under the NRHM
umbrella. The earlier RCH programme (RCH1) funded a fixed set of activities.
Under the NRHM, the earlier form of the RCH programme is being phased out. In
RCH2, most activities are funded through an RCH flexible pool which supports
decentralized planning and flexible programming by the states (NRHM, 2005). All
these show that NRHM includes many schemes covered under the CSS/CPS.
A study of expenditure on
different components of NRHM throws some light on the sustainability of earlier
programmes sponsored through CSS/CPS. The NRHM mission flexible pool, which
provides much of “new” funds to the states, accounted a higher amount and shows
increasing trends as per cent to GDP over the period, except for the recent
years. Its share in compositional term has also increased from 13.2 per cent in
2005-06 to 35.2 per cent in 2012-13. The RCH flexible pool, which provides the
greater flexibility to states spending on RCH related activities, has also
constituted higher amount and show increasing trends as per cent to GDP. In
compositional term its share increased from 17.6 per cent in 2005-06 to 26.4
per cent in 2012-13. The expenditure on maintenance of infrastructure however was
on high priority at the time of launch of NRHM. These components constituted
higher amounts as per cent of GDP in 2005-06 but started declining thereafter.
In compositional term, its share stood around half of the NRHM funds (about
46.9%) in 2005-06 but declined to 33.3 per cent in the year 2012-13. One of the
possibilities of decline in expenditure of these components is that central
government has allocated funds on condition that state governments need to
increase their own spending at a specified rate in tandem with the increased
central funding. Inadequate absorptive capacity of state governments probably
has come in the way that expenditure on these components has not been
increased. As regards to the programmes relating to NDCP, the expenditure from
these programmes, in composition term, declined significantly from 14.4 per
cent in 2005-06 to 4.5 per cent in 2012-13. Similar trends are reflected in
case of pulse polio programmes which raises question of sustainability of these
programmes. Therefore, it can be argued that overall increment in expenditure
on NRHM components is positive for health sector but the changing pattern of
health expenditure, through different routes raises issues of sustainability of
some of these programmes and has also made health expenditure more opaque. It
can also be argued that increased funds passing through state implementing
agencies were expected to improve the delivery system of health services in the
rural areas. The outcomes however do not show what was expected rather the
sharing of public health responsibilities between centre and states have made
the process even more cumbersome.
different components of NRHM throws some light on the sustainability of earlier
programmes sponsored through CSS/CPS. The NRHM mission flexible pool, which
provides much of “new” funds to the states, accounted a higher amount and shows
increasing trends as per cent to GDP over the period, except for the recent
years. Its share in compositional term has also increased from 13.2 per cent in
2005-06 to 35.2 per cent in 2012-13. The RCH flexible pool, which provides the
greater flexibility to states spending on RCH related activities, has also
constituted higher amount and show increasing trends as per cent to GDP. In
compositional term its share increased from 17.6 per cent in 2005-06 to 26.4
per cent in 2012-13. The expenditure on maintenance of infrastructure however was
on high priority at the time of launch of NRHM. These components constituted
higher amounts as per cent of GDP in 2005-06 but started declining thereafter.
In compositional term, its share stood around half of the NRHM funds (about
46.9%) in 2005-06 but declined to 33.3 per cent in the year 2012-13. One of the
possibilities of decline in expenditure of these components is that central
government has allocated funds on condition that state governments need to
increase their own spending at a specified rate in tandem with the increased
central funding. Inadequate absorptive capacity of state governments probably
has come in the way that expenditure on these components has not been
increased. As regards to the programmes relating to NDCP, the expenditure from
these programmes, in composition term, declined significantly from 14.4 per
cent in 2005-06 to 4.5 per cent in 2012-13. Similar trends are reflected in
case of pulse polio programmes which raises question of sustainability of these
programmes. Therefore, it can be argued that overall increment in expenditure
on NRHM components is positive for health sector but the changing pattern of
health expenditure, through different routes raises issues of sustainability of
some of these programmes and has also made health expenditure more opaque. It
can also be argued that increased funds passing through state implementing
agencies were expected to improve the delivery system of health services in the
rural areas. The outcomes however do not show what was expected rather the
sharing of public health responsibilities between centre and states have made
the process even more cumbersome.
Concluding Observations
The public expenditure on
health in India
is one of the lowest amongst the many developing countries and from the international
standard of spending. A low level of government spending on health sector seems
to be a generic problem in India.
The individual states were also unable to meet even the minimal level of
resource requirement for maintaining/ providing the basic health facility in
the country. It has been realised that neither centre nor the state governments
have ever fulfilled their commitment of health spending. This has resulted in
inadequate provisions of health facility in the country, e.g., bed: population
ratio in India
is 1:1000 compared to the 7:1000 in developed nations. This has further
resulted in high (71%) out-of-pocket spending which is met out from
individual’s pocket.
health in India
is one of the lowest amongst the many developing countries and from the international
standard of spending. A low level of government spending on health sector seems
to be a generic problem in India.
The individual states were also unable to meet even the minimal level of
resource requirement for maintaining/ providing the basic health facility in
the country. It has been realised that neither centre nor the state governments
have ever fulfilled their commitment of health spending. This has resulted in
inadequate provisions of health facility in the country, e.g., bed: population
ratio in India
is 1:1000 compared to the 7:1000 in developed nations. This has further
resulted in high (71%) out-of-pocket spending which is met out from
individual’s pocket.
The expenditure on health however
shows little increasing trends especially after the implementation of NRHM in
2005. But spending level (1.2 per cent of GDP) recorded lower than the ambitious
commitments of increasing in the government health spending to 2-3 per cent of
GDP by the end of 11th plan. Under the mission, the central
government however has asked the state governments to increase their own
spending at a specified rate in tandem with the increased central funding. The
state governments however did not increase their spending at the required
level. Therefore, the transfer of central funds to state, which was based on
some conditionality, could not be utilized by the state governments adequately.
This is being reflected by the inadequate absorptive capacity of state
governments to utilize funds properly, which further result in slowing down the
NRHM implementation. Probably, lack of availability of human resources, weak
capacity to plan and their execution probably limits the state governments to
absorb the central fund adequately.
shows little increasing trends especially after the implementation of NRHM in
2005. But spending level (1.2 per cent of GDP) recorded lower than the ambitious
commitments of increasing in the government health spending to 2-3 per cent of
GDP by the end of 11th plan. Under the mission, the central
government however has asked the state governments to increase their own
spending at a specified rate in tandem with the increased central funding. The
state governments however did not increase their spending at the required
level. Therefore, the transfer of central funds to state, which was based on
some conditionality, could not be utilized by the state governments adequately.
This is being reflected by the inadequate absorptive capacity of state
governments to utilize funds properly, which further result in slowing down the
NRHM implementation. Probably, lack of availability of human resources, weak
capacity to plan and their execution probably limits the state governments to
absorb the central fund adequately.
Another feather of NRHM was to
transfer some of the central funds, which were earlier routed through state’s
budget (through Centrally Plan and Sponsored schemes-CPS/CSS) are now
transferred to states through state implementing agencies which bypass the
state’s budget. This changing route of central transfer has put limitations on
certain central sponsored health programmes running through CPS/CSS. It was
noticed that central transfer through CPS/CSS were declining which results in discontinuity of some of the
health programmes running in the villages like the pulse polio and national
disease control programmes. This bypassing nature of central transfer can
probably lead to disincentives to mobilize funds from state’s own exchequer. The
states might think that NRHM is a financial responsibility of central
government. Secondly, it is difficult to monitor the central funds passing
through state implementing agencies and see whether these funds have been
implemented effectively at the ground level. Further, with this changing route
of central transfer, the financial relationship between centre and state in a
federal structure becomes unnecessarily complex.
transfer some of the central funds, which were earlier routed through state’s
budget (through Centrally Plan and Sponsored schemes-CPS/CSS) are now
transferred to states through state implementing agencies which bypass the
state’s budget. This changing route of central transfer has put limitations on
certain central sponsored health programmes running through CPS/CSS. It was
noticed that central transfer through CPS/CSS were declining which results in discontinuity of some of the
health programmes running in the villages like the pulse polio and national
disease control programmes. This bypassing nature of central transfer can
probably lead to disincentives to mobilize funds from state’s own exchequer. The
states might think that NRHM is a financial responsibility of central
government. Secondly, it is difficult to monitor the central funds passing
through state implementing agencies and see whether these funds have been
implemented effectively at the ground level. Further, with this changing route
of central transfer, the financial relationship between centre and state in a
federal structure becomes unnecessarily complex.
The overall analysis confirms
that India
and its states are shying away from fulfilling its constitutional commitment of
‘Right to Health’ for its citizens. We observed that public health sector has
never been given adequate resources to perform well in India. Given
the low level, declining and fluctuating behaviour of health expenditure over
the last twenty five years, it is not surprising that the health sector
performance had not been satisfactory. The failing nature of better health
outcomes however can easily be reversed with increased allocation in this
sector. Specifically, India
needs to double or triple its health spending from its existing level. Along
with the commitments of health spending, it becomes important to ensure that
the allocated additional public funds get spent effectively across its
constituent states.
that India
and its states are shying away from fulfilling its constitutional commitment of
‘Right to Health’ for its citizens. We observed that public health sector has
never been given adequate resources to perform well in India. Given
the low level, declining and fluctuating behaviour of health expenditure over
the last twenty five years, it is not surprising that the health sector
performance had not been satisfactory. The failing nature of better health
outcomes however can easily be reversed with increased allocation in this
sector. Specifically, India
needs to double or triple its health spending from its existing level. Along
with the commitments of health spending, it becomes important to ensure that
the allocated additional public funds get spent effectively across its
constituent states.
The
author is Assistant Professor at the Institute for Studies in Industrial
Development, New Delhi.
author is Assistant Professor at the Institute for Studies in Industrial
Development, New Delhi.