Shantanu De Roy
Shantanu De Roy
Introduction
After more than two months of lockdown, when the union and various state governments have decided to initiate economic activities, albeit in a controlled manner, it is still not clear how well the health care system in India is prepared in dealing with the pandemic. A pandemic of this magnitude requires a robust health system with combined initiatives from the public and private sector involved in health care. However, rapid spread of infections and disease and socio-economic profile of large sections of the populace necessitates strengthening of the public health care system in India that can meet this health challenge and provide cheap and quality health care to substantial sections of the citizenry. In this scenario, it is essential that the union and state governments allocate more resources for the public health system in India. However, since Independence, except for one or two states, development of health care has been neglected primarily due to inadequate allocation of resources. While it is argued that the lockdown phase should be used to revamp the health system in India, yet, given past trends, there is little hope.
This article argues that lack of development of health care, largely due to inadequate allocation of resources, is inextricably related to the trajectory of development in India since Independence.
Genesis of Public Provisioning of Health care in India: Recommendations of Bhore Committee
The first serious attempt at creating a public health system in India was made by the colonial administration, almost at the end of its rule in India, with the formation of Health Survey and Development Committee, under the chairpersonship of Joseph Bhore. The Committee was formed in 1943 and it submitted recommendations in 1946. It needs to be noted that the constitution and recommendations of Bhore Committee were consistent with the then prevailing discourses in the United Kingdom in creating a health system under active state intervention. The Committee argued for creating a three-tier organisation of health care—primary, secondary and tertiary care to strengthen the public health system in India. The Committee also recommended allocating 15 per cent of the total value of output on health care.
Unfortunately, most of the recommendations of Bhore Committee, remains unfulfilled even to this date, after 70 years of Independence. These recommendations were radical, since there was no health system and the country had inherited a huge disease burden from almost 200 years of colonial rule.
Post-Independence Development Trajectory in India: A Saga of Compromises
Even though the Congress Planning Committee considered health as a basic human right, yet, compromises were made immediately after Independence in which right to health was relegated into the Directive Principles of State Policy. Thus, rights-based approach accessing health care in India was negated by the policy makers immediately after Independence. In contrast to the recommendations of Bhore Committee that argued for creating a health system, the government was more focused in family planning and reducing loss of human lives from infectious diseases like malaria, tuberculosis and small-pox. As a result, efforts to create a health system—an organisational set-up of health care—suffered a setback. Notwithstanding their admiration of the Soviet planning model, policy makers in practice followed a mixed economy framework after Independence. An important objective of the state led capitalist development was to promote accumulation process of a small section of urban and rural bourgeoisie.
In the rural areas, compromises with the landed sections was reflected in failed attempts to alter agrarian relations through institutional reforms. Moreover, agricultural incomes were kept out of the tax net. These compromises had (a) failed to alter correlation of class forces in the countryside in favour of the rural and working poor (b) market for mass consumption goods remained narrow leading to excess capacity in the industrial sector, and (c) adversely affected capacity of the state to mobilise adequate resources since agricultural incomes were exempted and excise taxes suffered due to excess capacity in the industrial sector. The resultant fiscal burden forced the state to reduce expenditures on crucial social sectors like education and health.
Among the urban bourgeoisie, institutionalization of the Hindu Undivided Family (HUF) as a form of property holding have been instrumental in terms of reducing the tax liability of the big business of Hindu origin that have, in turn, adversely impacted government revenue mobilisation. Through these measures the state had enabled concentration of land and non-land resources among a small section of population in India that are excluded from the tax-net. Although Nehruvian model of state led capitalism led to increased production as compared to the colonial period, it did not lead to structural transformation of the economy. In other words, continued dependence on agriculture, which was outside the tax regime, as a major source of employment and income had put brakes on resource mobilisation by the state.
Further, landed sections in the agrarian economy, following the benefits from green revolution, diversified into non-agricultural sector including health care. Inadequate allocations of resources meant that the public health care was inadequate in meeting health needs of the population. Additionally, quality of health care of public sector was compromised. Increasing demand for health care was met by successive governments through reduction of tariffs on imports of medical equipment to facilitate the growth of private sector in health care; similar concessions were provided to the NRIs. Since the 1980s, the emerging salaried middle-class that had achieved a reasonably adequate standard of living following implementations of Pay Commission recommendations, started to lobby for hi-tech and super-specialty hospitals which conformed to international standards of health care whose needs were met by a rapidly growing private sector.
The resultant fiscal crisis due to failure to mobilize adequate resources through progressive direct taxes meant that the growth process had to be dependent on resources mobilized through indirect taxes, thereby leading to erosion of purchasing power on large sections of the workers and squeezing the demand and narrowing the domestic market further. Reduction of taxes on economic surpluses of major private entities and/or increase in transfers by way of tax concessions and subsidies from the public to private sector adversely affected public spending. According to the Indian Public Finance Statistics database, tax-GDP ratio in 1950-51 was 6 per cent and the share of direct taxes in total tax was marginally more than a third (37 per cent); in 1989-90, tax-GDP ratio was 15.5 per cent and the share direct tax in total tax collections declined to 14.6 per cent.
As a result, the share of public expenditure on health in GDP in India did not exceed 1 per cent during this period. Share of public expenditure in total expenditure on health among selected nations at a comparable level of development was lowest in India after 40 years of planning in 1990 (Figure 1).
Figure 1: Share of public expenditure in total expenditure on health (in per cent), 1990
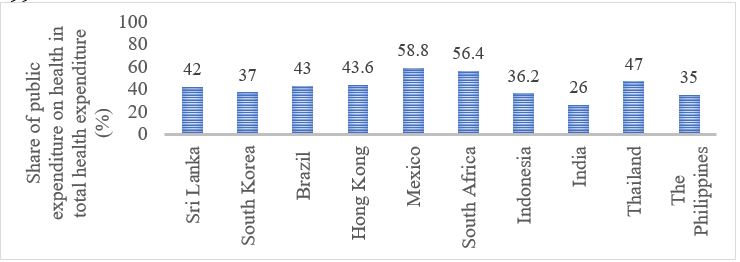
Note: Data for Brazil, Indonesia and The Philippines are with respect to 1995; South Africa, 1987; India 1991 and Thailand 1994. This was done due to unavailability of data for the same year across nations.
Source: Sri Lanka Health Accounts, Health Systems in Transition (2011) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194835/ (South Korea), World Bank (2014) (Brazil), Liu and Yue (1998), Mcintyre et al (1990) (South Africa), Duggal (2007) (India), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194642/(Mexico), Asia Pacific Observatory on Health Systems and Policies (2017) (Indonesia), Lindelow, Magnus, Loraine Hawkins and Sutayut Osornprasop (2012) (Thailand).
Inadequate allocations adversely affected creation of health infrastructure under state initiatives. Bhore Committee’s expectations that a growing public health care system will reduce dominance of private practitioners did not materialise due to slow growth of government health care facilities on account of meager allocations. Inability of the government to control private practices of doctors employed in the public sector strengthened private interests. In this scenario, efforts by various state governments to regulate private sector, by banning private practices of doctors employed in government hospitals eventually led to failures. Eventually, as Qadeer (2008) noted, “the powerful private sector was able to join the pressure for ‘reforms’ and ‘international standards in medical care’ and carve a space for itself in the Government’s 1983 National Health Policy.” Mudaliar Committee—constituted in the early sixties—noted that the fiscal situation in India did not allow creation of a health service in line with the National Health Service in the United Kingdom. In view of the paucity of resources allocated for health care, the Committee recommended introduction of user fees to enable the state to improve quality and quantum of health care.
To sum, class bias of development trajectory pursued by the state during the first 40 years after the initiation of planning, in terms of providing tax incentives to a small section at the top of the economic and social hierarchy to further the process of accumulation, was largely responsible for inadequate government intervention in health care. While on the one hand, public health care system suffered, in terms of quality and reach, due to inadequate allocation of resources, tax concessions and subsidies provided to the private sector allowed them to grow significantly.
Post-reform developments: Chimera of Universal Health Care
Initial thirty years of Planning period—till the 1980s—was noted for policy documents and pronouncements in which role of the state in health care was crucial with the private sector carrying the mantle of a partner. That did not materialise due to compromises made by the state particularly in generating and mobilizing of resources. However, during the post-reform period, with neoliberalism emerging as the core ideological apparatus, minimum semblance of controlling the private sector in health care that existed in the policy documents, prior to reforms, was done away with. In complete contrast to the initial forty years of planning, the post-reform phase was marked by overall de-legitimisation of the public sector and the associated processes of relegating the role of the state to a facilitator to the private sector rather than a provider of health care.
Moreover, with the dis-integration of USSR and Socialist Bloc of Eastern Europe planning models across the world received a massive blow. Retreat of welfare state and social democracy were concomitant features. India was no exception to this global trend. In other words, the semblance of ‘human face’ of capitalism that was nurtured for almost 40 years was substantially eroded. Multi-lateral funding agencies, like the IMF and World Bank, started to dominate the WHO in policy level recommendations and argued for increasing private participation in health care which was reflected in the two important documents related to health care—the World Development Report in 1993 and Report of Commission on Macroeconomics and Health in 2001. In 2005, the WHO proposed the idea of Universal Health Care (UHC), that meant provision of financial support by the government for approaching health care providers—large sections of whom are private providers in the developing economies due to weaknesses of public health care system— and does not necessarily ensure provision of actual services.
These changes marked transition in health care in which successive governments has been gradually shifting its role from health care provider to purchaser and is concentrating more on demand pool strategies instead of supply side measures. Initiation of Government Funded Health Insurance Schemes (GFHIS), whereby governments purchase health care from providers is an outcome of such demand pool strategies.
Health care providers can either be private or public; insurance companies are by and large private entities. Recently, trust model of financing was initiated in which a government agency is the purchaser of health care services from private and public providers, often the latter, in a competitive market. Under this arrangement, the funding agency, public trust in this case, based on competitive bidding, purchases best quality health care at the lowest possible price. However, the domestic market of health care is increasingly characterized by concentration and centralisation of capital. It has been argued that global equity funds and their domestic partners, often in collaboration, have been acquiring relatively smaller hospitals in India (Chakravarthi et al, 2017). Easing of restrictions on global capital flows have facilitated accumulation of capital of the private sector in the post reform period. Also, dominance of private players among the health care providers and insurance companies has meant that profit motive invariably received more importance as compared to social welfare maximisation. As a result, India is noted for one of the highest out of pocket expenditures on health care among the developing nations (Figure 2). In India, burden of expenditure on health care is disproportionately borne by the poorest sections of the population. NSSO database suggest that the expenditure on health care as share in total consumption expenditure was 8 per cent on the poorest sections of the population; corresponding figure for the richest section was 6 per cent. The National Health Accounts, 2014-15 had estimated that two-third of the total health expenditure is from the out-of-pocket of citizens and it has become the dominant source of financing of health care in India. Recent reports suggest that the scenario is no different as far as the treatment of Covid-19 patients are concerned.
Figure 2: Out of pocket expenditure as share in total health expenditure across selected developing economies, 2000-2015 (in per cent)
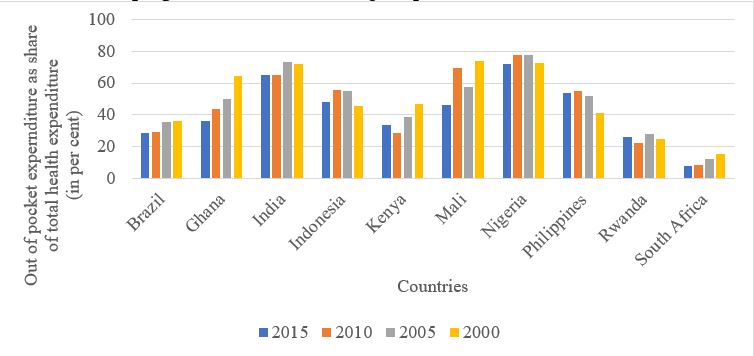
Source: World Bank database
Thus, government’s efforts in providing health care through the insurance/trust model has failed in realizing the most important objective of provide financial protection of the most vulnerable sections of the population. Hence, in the post reform period, increased intervention for health care by the union and state governments should focus on creating health infrastructures like hospitals and recruiting more doctors and other health professionals to strengthen the health system rather than furthering interests of private health care providers and insurance companies.
India needs a strong public health care system more than ever. However, the development trajectory pursued since Independence was inimical in terms of creating one, that can potentially lead to dangerous outcomes in the current context. In view of the health challenges posed by the pandemic, short-term measures may not be enough; what India needs is re-thinking its development framework for inclusive development of health care.
The author is Assistant Professor at TERI University