Pritam Datta and Chetana Chaudhuri
Pritam Datta and Chetana Chaudhuri
Death, disease and illness are unavoidable mortal attributes of the human race since its very beginning. There are more than a thousand known species of human pathogens and almost all of them are capable of causing outbreak locally as well as globally, if left unchecked. Plague, smallpox, influenza and cholera were some of the most brutal killers in the history of mankind. Every epidemic ravaged human lives and civilization but teaches some important lessons: the importance of clean water or better hygiene or community health. Today the world is facing struggle for existence after the global outbreak of COVID-19 and it is important to learn from this crisis.
As recommended by the structural adjustment programmes (SAP) of the World Bank, private sector has been encouraged to increase engagement with public healthcare providers over the past decades in developing nations like India. Countries around the world had changed their emphasis from state-based social security system for health to insurance-based mechanism, and India is not an exception. Federal as well as state governments in India are gradually entering into the bandwagon of government sponsored health insurance schemes (GSHIS) like ‘Pradhan Mantri Jan Arogya Yojana’ (PMJAY) or state sponsored health insurance schemes like Chief Minister’s Comprehensive Health Insurance Scheme (CMCHIS). At the same time Indian government is increasingly trusting on private sector as provider of health care and confined herself only as financier. Even the latest National Health Policy[i] (2017) has mandated purchase of selected benefit package of secondary and tertiary care services from private providers under Government sponsored health insurance schemes (GSHIS). Even recent federal budget (2020-21) emphasises on larger reliance on private sector for provision of healthcare; proposes both setting up new hospitals and attaching certain medical colleges to existing district hospitals in Private-Public Partnership (PPP) mode.
But, the role of private sector in delivering healthcare is a debatable issue. Health care market is characterized by a high degree of uncertainty. A provider may influence and induce the patient’s demand for care beyond the required, optimum or cost-effective level, especially when there is a clear linkage between service volume and profits associated with fee-for-service payment mechanism. Private for-profit providers may be motivated by making money at patient’s expense and in that case, profit motive might override good clinical practice of contributing in larger public health goals of the nation.
Figure 1: Utilization of public and private hospitals in inpatient and outpatient healthcare
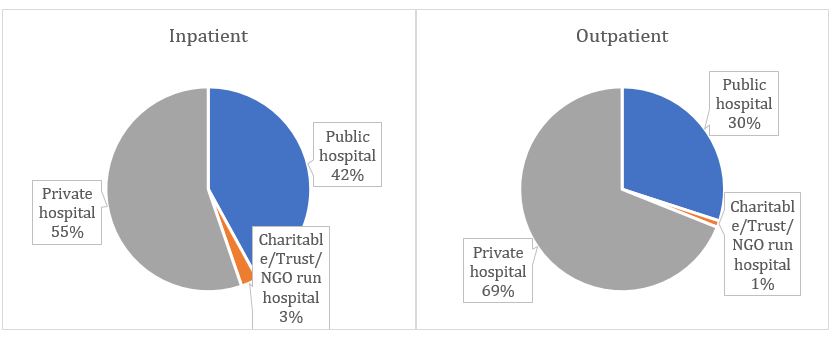
Source: Author’s estimation from unit level 75th round NSSO data
According to latest available survey data on Social Consumption of Health in India conducted by National Statistical Office (NSO) in 2017-18 (75th Round), majority of hospitalization cases (58%) in India are treated in private sector and for outpatient treatment, the share of private sector is even higher (Figure 1). However, average treatment cost is five and seven times higher in private not for profit charitable and private for profit commercial hospitals as compared to public providers in India. Similar trend is followed in outpatient care too (Table 1). Both for diagnostic and medicine, private sector charges on an average are around 3 to 4 times higher as compared to public sector for IP care. Bed charges and consultation fees for IP care in private hospitals are 29 times and 32 times higher in private sector as compared to public sector[ii].
Table 1: Comparison of per episode treatment cost (INR) in Public and Private Facilities
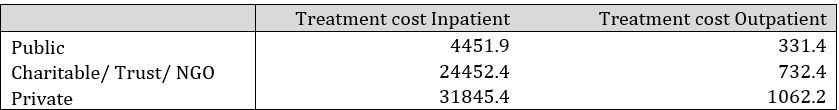
Source: Author’s estimation from unit level 75th round NSSO data
The processes and authorities of registration of private providers differ across states and even generating a comprehensive list of private providers across the country is difficult (Choudhury & Datta 2020)[iii]. There is a dearth of detailed data on corporate hospitals in public domain. Even today in absence of sufficient numbers of government facilities, India needs to allow private sector to charge up to Rs 4,500[iv] per test for COVID-19, while that is free at government facilities. The Supreme Court mandated[v] government to make COVID-19 testing at private sector free for poor and vulnerable. India’s cost for COVID-19 test is highest[vi] in South Asia. It is important to note here, that the patients are discharged only after 3 to 5 consecutive tests (Rs. 4500 for each) turn negative.
Majority (80%) of the COVID-19 patients are treated in public hospitals in India[vii]. The cost of treatment of COVID-19 varies significantly, depending on the load of virus, other morbidities, age, immunity of the patient and other factors. It is reported that some private hospitals are charging around Rs. 4.8 lakh for the treatment of COVID-19 for 9 days or even Rs. 15 lakh for a stay of one month in hospital[viii]. For the patients who needed ventilators were charged Rs. 80,000 per day for a ventilator. The exorbitant charge worsens the situation when 50% of the hospital charges was for PPE kits, N95 masks and shields, which insurance companies refuse to reimburse[ix]. It is noteworthy that only a handful of people are under insurance coverage, risking the vulnerable population into impoverishment and catastrophic health expenditure. In a situation, when health system is clearly shifting from public to private and the government is promoting insurance-based healthcare system, it raises serious concern about the inclusiveness of poor and vulnerable in our country’s healthcare system.
The pandemic exposed the feeble condition of public health system in India. Moreover, it is clearly realised that public health system needs to be in the forefront in crisis situation like today. At the policy level, India has rolled out Universal Health Coverage (UHC) in its 12th Five-year plan (i.e. 2012-17) but even now out-of-pocket spending on health care holds the largest part in total health care spending in India. Federal government[x] spends roughly 11% of total health care spending of the country.
Figure 2: Federal spending on Indian Health Care
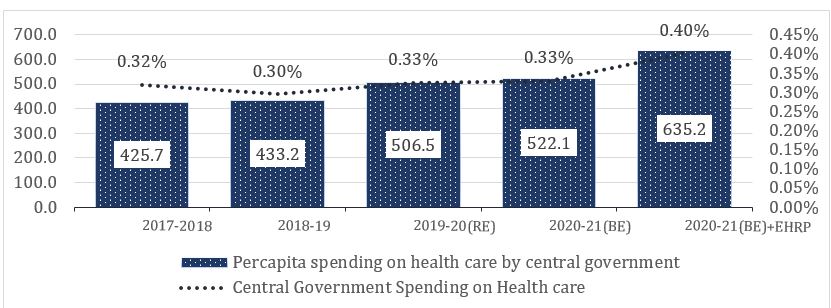
Source: Union Budget 2020-21 and ABA documents in PIB releases
Government of India recently announced its economic package-Atmanirbhar Bharat Abhiyaan (ABA) to reboot the economy. But unfortunately, health remains a neglected topic in this package too, as it was in previous federal budgets. Government of India announced an allocation of Rs. 69.2 thousand crores for the healthcare sector in the 2020-21 Union Budget, which is equivalent to 0.33% of Indian GDP and 2.3% of total federal budgeted expenditure in 2020-21. Under the Atmanirbhar Bharat Abhiyan, government of India announced ‘Essential Health Relief Package‘ (EHRP) of Rs. 15 thousand crore along with a long list of promises to increase public expenditure and investments in Public Health, building hospitals for infectious diseases at all districts, strengthening of lab network and surveillance as well as encouraging research. But no clear road map or budget allocation is outlined under ABA, till today. Figure 2 shows the federal spending on health care in India remains less than 0.5% of GDP even after incorporating additional amount budgeted for public health under ABA. The EHRP is providing only an additional relief of INR 113.1 per-capita to be spend on health care under the current public health emergency situation during 2020-21. India’s total public spending (taking federal and state governments together) is 0.96% of GDP and federal government contributes 32% of total public expenditure on health care. It is quite worrisome to note that public spending on health care as a percentage share of GDP in India is far less than the world average, even lower than that of low income countries (Figure 3).
Figure 3: Government Health Expenditure as % of GDP

Source: World Development Indicators (for the year 2017), The World Bank
The pandemic has opened up gaps in global health system led by private sector and the existential need of a robust public healthcare system came to the forefront in a glaring way. In the wake of the current pandemic we saw that it is the public health care system that has expanded and accommodated the surge of critically affected patients around the globe. The participation of private health care providers, at least in the initial phase of the pandemic was negligible and that is clearly not affordable for majority of the population. Thereby, India needs to upscale its public health expenditure to strengthen its public health care system across the country to manage today’s crisis in a better way, to be prepared for such shock in future as well as to control supplier-induced inflationary pressure on health care system of the country.
Pritam Datta is Fellow (II), National Institute of Public Finance and Policy (NIPFP), New Delhi
Chetana Chaudhuri is Senior Research Associate, Public Health Foundation of India (PHFI), Gurgaon
[i] National Health Policy (2017), Ministry of Health and Family Welfare, Government of India
[ii] https://www.epw.in/journal/2020/22/commentary/role-private-sector-escalating-medical-inflation.html#
[iii] https://www.epw.in/journal/2020/17/special-articles/health-insurance-private-hospitals.html
[iv] https://www.bbc.com/news/world-asia-india-52322559
[v] https://caravanmagazine.in/health/india-private-covid-19-tests-cost-highest-in-south-asia-free-in-bangladesh
[vi] https://caravanmagazine.in/health/india-private-covid-19-tests-cost-highest-in-south-asia-free-in-bangladesh
[vii]https://www.hindustantimes.com/india-news/what-does-it-cost-to-treat-a-coronavirus-patient-here-s-a-break-up/story-qwOzwoaJKj39AAxb2U58oO.html
[viii] https://theprint.in/health/patients-say-delhi-pvt-hospitals-charging-huge-ppe-fees-hospitals-say-its-within-norms/432972/
[ix] https://www.indiatoday.in/india/story/coronavirus-treatment-cost-private-hospitals-ppe-n95-masks-india-1683567-2020-05-30
[x] http://nhsrcindia.org/updates/national-health-accounts-estimates-india-2015-16