Farhat Hossain

In the year 2005, The National Rural Health Mission (NRHM) was launched to strengthen the rural health services and proper financial management. The health care services in urban areas with a population of more than 50000 are covered by the Nation Urban Health Mission (NUHM). The National Health Mission (NHM) was initiated in the year 2013 by including NRHM and NUHM. The NHM mainly funded by the central government and implemented through the concept of decentralized governance of health services. The major development under NHM was the transfer of Flexi pool fund directly to the different states (State Health Societies) in the country and to the respective district health societies (Narwal, 2015). The decentralized structure of health societies are executed at different levels and units of governance like State, districts and blocks. The fund sharing ratio of the central government to the state government is 60:40. Firstly the funds are released by the central government to the State health Societies (SHS) then SHS release it to the District health societies (DHS) and the corresponding lower-level units. It is mention in the operating manual of NHM (2013) that at least 70 percent of funds should be allocated to the districts and high priority districts allocated 30 percent more of funds. Other than this, the district with tribal and vulnerable population should be given special attention. But if we travel through district-level funding in West Bengal it gives reverse trends.
.
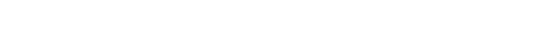
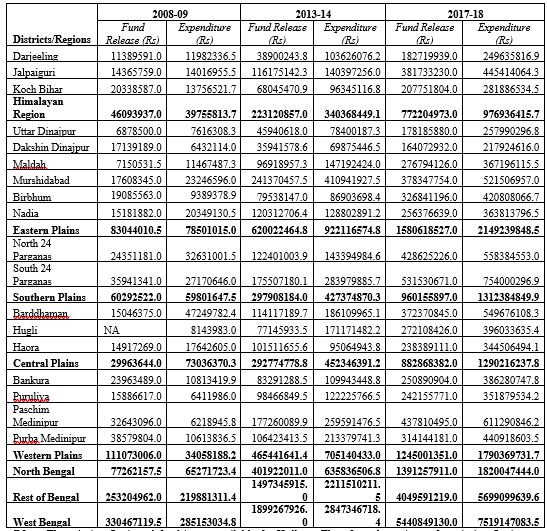
The higher proportion of scheduled caste and scheduled tribe population resides in North Bengal. The districts of Jalpaiguri and Cooch Behar are having highest concentration of scheduled caste population with 37.65 percent and 50.17 percent respectively. The highest proportio of scheduled tribe population are found in the district of Darjeeling with 21.52 percent followed by Jalpaiguri (18.89 percent) and Dakshin Dinajpur (16.43 percent). The religious distribution is quite different in North Bengal. The Maldah and Uttar Dinajpur are identified as minority concentration districts of category A with 49.72 percent and 47.36 percent of the Muslim population. The other two districts i.e. Cooch Behar and Dakshin Dinajpur also belong to category A of Muslim minority with 23.34 percent and 24.2 percent respectively. It is evident from the ICSSR project (2008) on minority concentration districts that the levels of development in accessing the basic services was very poor and unfortunately have glaring disparity. These four districts are relatively deficient in terms of amenities and services and also suffer from the continuous process of underdevelopment. The major challenges of health system is to strengthen and implement the goals defined in NHM fund as per the norms and allocate to district and block level health governance. The mission flexi pool fund of release and expenditure under NHM is shown in table 1. The fund release was quite high for the western plain region in the year 2008-09 and then it followed by eastern plain and southern plain region. In the year 2017-18, the fund release is higher for eastern plain region and followed by western plain and southern plain region.
.
It is very surprising fact that southern plain consist of two districts i.e. North and South 24 Parganas and the proportionate share of fund release was quite high for these two districts in comparison to other districts of West Bengal.On the other side, Purbo and Paschim Mednipur district of Western plain region have higher share of fund release as compared to Bankura and Purulia district of Western Plain region.North Bengal shares 23.38 per cent out of the total fund release of the state as compared to 33.61 per cent of western plain region in the year 2008-09. Over the period of time (2008-09 to 2017-18), the fund release is increased for North Bengal by 1.89 per cent.The district wise fund release is quite low for Uttar Dinajpur and Dakshin Dinajpur and it is highest for North 24 Pargana, South 24 Pargana and Paschim Mednipur. Although, Uttar Dinajpur, Kochbihar and Malda are the high priority districts as per NHM goals and also have vulnerable population. But it did not receive sufficient attention by the State Government and these districts are also known as migrant labour concentrated areas. It is clearly depicted in the table 1 and 2 that there are regional disparity in terms of fund release by the state.
It is very surprising fact that southern plain consist of two districts i.e. North and South 24 Parganas and the proportionate share of fund release was quite high for these two districts in comparison to other districts of West Bengal.On the other side, Purbo and Paschim Mednipur district of Western plain region have higher share of fund release as compared to Bankura and Purulia district of Western Plain region.North Bengal shares 23.38 per cent out of the total fund release of the state as compared to 33.61 per cent of western plain region in the year 2008-09. Over the period of time (2008-09 to 2017-18), the fund release is increased for North Bengal by 1.89 per cent.The district wise fund release is quite low for Uttar Dinajpur and Dakshin Dinajpur and it is highest for North 24 Pargana, South 24 Pargana and Paschim Mednipur. Although, Uttar Dinajpur, Kochbihar and Malda are the high priority districts as per NHM goals and also have vulnerable population. But it did not receive sufficient attention by the State Government and these districts are also known as migrant labour concentrated areas. It is clearly depicted in the table 1 and 2 that there are regional disparity in terms of fund release by the state.
Table-1: District/Region wise Mission flexi pool Fund Release and Expenditure under NHM
Note: The mission flexi pool fund is not available for Kolkata. Therefore, the estimate for mission flexi funds of Southern Plain region composed of two districts only i.e. North 24 Parganas and South 24Parganas]
.
Source: Computed from Unpublished data Collected by the Researcher from Govt. of West Bengal
.
Table 2: District/Region wise Proportionate Share of Mission flexi pool Funds Release and Expenditure under NHM
.
Inadequate Health Care System in North Bengal
There are insufficiencies of rural health infrastructure in North Bengal to treat majority of the rural patients and not fulfilling the norms of NHM (see Fig 1). The average population served per rural health care institution are very high in North Bengal as compare to rest of Bengal. Although, the population density is low in the districts of North Bengal with 804 persons per sq.km as compare to 1029 persons per sq. km in West Bengal (Census, 2011). Average population served per PHC, BPHC and rural hospital beds are quite high in North Bengal as compared to the state average and rest of the Bengal. Average population served per BHC beds in North Bengal 87457 persons in comparison to 51604 persons in West Bengal. The corresponding figure for PHC and rural hospital beds in North Bengal are 11267 and 7307 persons in contrast to 8919 and 6643 persons in West Bengal (Health on March 2015-16). It is reported in Uttarbanga Sambad (26.03.2020; 31.03.2020 and 05.04.2020) that there are lack of resources in the government hospitals to deal with Covid-19 crisis. The health care institutions reported the facts before media and accepted the limitations to tackle the COVID-19 crisis due to the limited availability of health manpower, equipment, masks, sanitizer, Personal Protection Equipment (PPE) kit and insufficient health infrastructure.
.
Fig -1: Health Infrastructure under NHM and Institution of Governance

Source: Cited from NHM PIP operative manual, MOHFW, GOI
.
Governing Health and Outcomes in North Bengal
The state of West Bengal is unique in the country where left government ruled for more than a quarter of a century. The two major public initiatives had implemented by West Bengal Government in 1977 was land reforms and decentralisation which impacted positively in reducing poverty, and in the process of growth and development of the State. However, it is evident from various literature (Raychoudhuri and Haldar, 2009 and Purohit, 2008) and government reports (WBHDR, 2004; Planning commission, 2002) that the inter-district and intra-regional differences in the state are widening. The six northern districts are considered as backward region due to the insufficient socio-economic outcomes and lack of infrastructure facility.
.
Other than this the process of decentralisation is also very poor in the districts of North Bengal. The evolution report of the Department for International Development (DFID) of Strengthening Rural Decentralisation (SRD) programme identified that these priority districts requiring more focus intervention and need planning on poverty. It is also found that the Fiduciary Risk Assessment (FRA) was also high in these districts. As per the Annual Administrative Report (2008-09), Panchayat and Rural Development Department, Govt of West Bengal, most of the districts in North Bengal are the worst-performing districts in terms of service delivery by the panchayats of the respective districts. The literature on decentralisation of service delivery suggests that local-level democracy may not function well due to unequal distribution of assets, literacy, social status and political participation. The poverty alleviation effort of the West Bengal panchayats was not achieved successfully due to the phenomenon of limited accountability of gram panchayats in the presence of high inequality in socioeconomic status and political power (Bardhan and Mookerjee, 2003).
.
As per the NHM manual there should be certain committees like Rogi Kalyan Samiti (RKS) at the district and block level and people’s organization such as Village Health Sanitation and Nutrition Committee (VHSNC) at gram panchayat level (See Fig-1). These committees are needed for decentralized outcome based planning and implementation. But these types of committees are not functioning properly as per the NHM guidelines. The Rogi Kalyan Samiti or patient welfare committee is an effective management structure for proper functioning and management of the hospital. The main objective of the RKS is to ensure proper accountability of public health providers to the society, proper availability of essential drugs, proper scientific disposal of hospital waste, provide drinking water subsidized food, medicine and cleanliness, introduce transparency in the management of funds, supervise the implementation of National Health Programmes, display of citizen charter, upgrade and modernize health service facility and undertake construction and expansion of building as per the hospital need (GOI, 2015).
.
The Rogi Kalyan Samiti is functioning at the district level only. At the block level, RKS is ineffective to address the various objectives. It is found from my fieldwork in the districts of Darjeeling and Uttar Dinajpur that only two meeting were conducted during six months at the block level. There are absences of activities between the Village Health Sanitation and Nutrition Committee (VHSNC) and the sub-centre in North Bengal region. During my field visit, it was found that all the interacted ANM and ASHA workers were not aware of the constitution of Village Health Sanitation & Nutrition Committee and it’s functioning. ASHA workers were unaware about their membership in the VHSNCs. The ANM and ASHA workers are not aware of the role of VHSNC and refer it as a function of Panchayat Samiti (Block Political Unit).
.
Conclusion
Within this backdrop, it is very important to promote institutionalization of panchayat raj with functions like health, finance and functionaries. The Committees like Rogi Kalyan Samiti (RKS) and Village Health Sanitation and Nutrition Committee (VHSNC) is the important instrument towards facilitation of inter-sectoral coordination, local community participation in decision making and improving facility based health care services (Narwal, 2015). But recently, State government announces withdrawing of power from the Rogi Kalyan Samities and makes it more centralised to overcome the present crisis (ABP Ananda report on 9/04/2020). The centralized system of health administration is creating more problems to deal with the COVID-19 crisis in rural populace of North Bengal. It has been already predicted by many researchers and scientists that the villages may become the hotspot of the disease after lifting the 21 days lockdown (The Hindu dated 09/04/2020). The Government of West Bengal identified seven hotspots in the states which include Egra, Howrah, Tehatta, Eastern Command Hospital (Kokata), Haldia, Kolkata, and Kalimpong. About 15 cases of COVID-19 are getting treated in North Bengal Medical College and Hospital (NBMCH) and Dr. Chang’s Private Hospital in Matigara. But it is very surprising fact to the people of North Bengal that the Siliguri town and adjoining areas are not identified as Hotspots of COVID-19 though both the NBMCH and Dr. Chang’s Hospital are situated in Siliguri only. This pandemic requires more engagement of panchayats with the collaborative effort of self-help groups to set up quarantine facilities within the village premises and provide masks, sanitizer, food and safe drinking water to the vulnerable populace and migrant labourers. During this health crisis Government should promote Mobile Health Services in the inaccessible terrain of North Bengal which include the facility of doctor, lifesaving medicines and diagnostic testing kits.
.
The author is a Ph.D Scholar, Special Centre for the Study of North-East India, Jawaharlal Nehru University, New Delhi. Any comments or suggestions can be sent over email at farhat.hossain88@gmail.com
.
References:
Bardhan and Mukherjee (2003), ‘Poverty Alleviation Effort of West Bengal Panchayats’, Mac Arthur Foundation, MIT, Pennsylvania State University, Stanford and Toulouse, pp.1-19.
.
Government of India (2013), National Health Mission (NHM) Draft Operating Manual for Preparation and Monitoring of State Programme Implementation Plans (PIPs), Ministry of Health and Family Welfare, New Delhi, PP-1-30. Available at https://palliumindia.org/cms/wp-content/uploads/2014/01/NHM_PIP_operating_manual_29.10.2013.pdf
.
Government of West Bengal (2016), Health on the March 2015-16 (Draft Copy), West Bengal, State Bureau of Health Intelligence, Directorate of Health Services, Government of West Bengal, Kolkata.
.
Government of West Bengal (2011), Annual Administrative Report (2008-09), Panchayat and Rural Development Department, Writers Building, Govt of West Bengal, Kolkata.
.
Government of West Bengal (2004), West Bengal Human Development Report, 2004, Development and Planning Department, Kolkata, West Bengal, pp.1-205.
.
Government of India (2002), Report on Comparatives Backwardness of North Bengal Region, Planning Commission, Institute of Applied Manpower Research, I.P.Estate, Mahatma Gandhi Road, New Delhi.
.
Narwal, R (2015), ‘Success and Constraints of the National Rural Health Mission- Is there a Need for Course Correction for India’s Move towards Universal Health Coverage?’ Social Development Report 2014, Council for Social Development, Oxford University Press, New Delhi, pp. 124-137.
.
Purohit, C. B. (2008), ‘Efficiency of The Health Care System: A Sub-State Level Analysis for West Bengal (India)’, RURDS, Vol.20, No.3, pp.212-225.
.
Raychoudhuri.A and S.K.Haldar (2009), ‘An Investigation into the Inter-district Disparity in West Bengal (1991-2005)’, Economic and Political Weekly, Vol. XLIV Nos.26 & 27, pp.258-263.
.
Sonubal, I.V (2020), ‘A key arsenal in rural India’s pandemic fights’, The Hindu, 09 April 2020, (Available at https://www.thehindu.com/opinion/lead/a-key-arsenal-in-rural-indias-pandemic-fight/article31293099.ece).
.
PTI (2020), Don’t Have adequate infrastructure to tackle COVID-19 crisis –Thought by Health Officials (Translated from Bengali), Uttarbanga Sambad, 26 March 2020, Siliguri, p-4
.
PTI (2020), Don’t Have Sufficient Equipment-Admitted by Health Officials (Translated from Bengali), Uttarbanga Sambad, 31 March 2020, Siliguri, p-3
.
Ghosh, R (2020), Improper arrangements for Infected Patients-Absence of Doctors, Lack of Resources (Translated from Bengali), Uttarbanga Sambad, 5 April 2020, Siliguri, p-1
.
ABP Ananda (2020), Swasthy Daptar can only take decision and withdrawing of power from Rogi Kalyan Samiti, ABP Ananda Television Network, 9 April 2020 Available at https://bengali.abplive.com/